for
Individuals
Better Quality of Life
Learn More
Resource

In March of 2004, I was driving in the car, feeling like I finally had a moment to myself, when I got a frantic call from my mother’s hospital doctor telling me my mother was in a code blue. “Do you want us to resuscitate her?” he asked. I remember thinking “of course!” and replying, “Yes, I’m on my way.” I began shaking all over and drove like a bat out of hell to the hospital.
At the time, I was running a part time business, had 2 young daughters and was overseeing the care of my mother who had dementia, among other major ailments. My mom had been in the hospital since when they took out her remaining kidney, which had developed a “nasty cancer.”
It was 2002 when my mother’s early dementia first became apparent, when I noticed a lot of past due notices on her desk. When I offered help by taking over her bills, she was visibly relieved and gladly pushed the pile my way. I also discovered she had been falling asleep during sessions with her private practice clients. Her medications were strewn all over the counter, and she didn’t seem to recall if she had taken them or not.
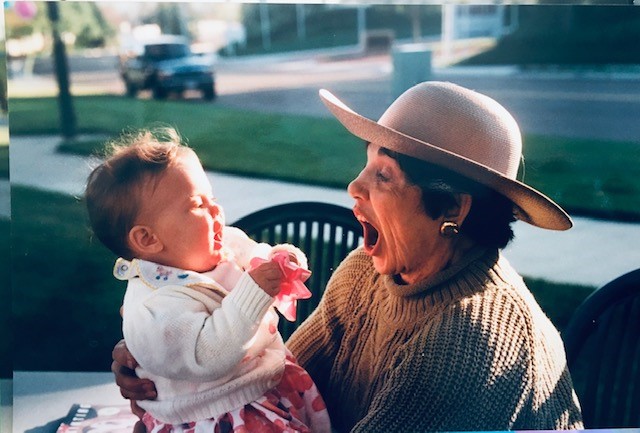
She stopped seeing clients and spent increasing amounts of time in her comfy chair watching television, often dozing. She insisted on staying in her own home. I would drive the 2 miles to her house three times a day to make sure she took her kidney transplant anti-rejections drugs, as scheduled. Many days were spent going to a variety of doctors’ visits. I had to give up my photography business in order to help my mother.

The Importance of Medical Guidance for a Caregiver- Knowing What to Expect
Over time, she began developing a variety of infections and UTI’s which caused her mental status to decline and make her “loopy.” It was over a year before a neurologist finally explained to me that when someone with dementia gets an infection, this is the normal response.
I found the hospital to be a confusing system. I had no idea who to ask for what or how to reach any of the doctors, who seemed to change every day and come in to visit at odd, unpredictable hours.
Hospitalization, nursing home for rehab, home, and back to the hospital became a loop that continued for the last two years of her life.
During that last long hospitalization, a doctor came in and sat by my mom’s hospital bed to talk with us. I was surprised by this doctor’s approach and all the time he spent with us that day. This doctor asked my mother about her goals of care and what she wanted for treatment. He talked about what it meant to be a DNR, do not resuscitate. I was so appreciative of how kind and gentle he was with my mother. However, it really was too late to ask her these types of questions. She was so confused, was wringing her hands and kept saying, “I’m not sure what I should do. I really don’t know.”

First-Time Advanced Directive Conversations and What May Be Missed
I vaguely recall at one point my mother showed me her advanced directive, but I didn’t pay close attention to which healthcare decisions she made. I don’t remember having much of a conversation with her at the time, and I didn’t really feel comfortable with the whole topic. Who wants to think about their mother dying? I figured she’d tell me what she wanted and if I needed the form at some point, I’d look for it.
Even though my mother had completed an advanced directive many years before, it only addressed her not wanting resuscitation if she would not be able to recover. She still chose to be resuscitated if she had a chance. It was not a full picture of the Advance Care Plan, it didn’t address the grey areas like:
Even though she was a psychotherapist, we had never had these types of conversations. I really didn’t know what she wanted. Years before she would joke and say, “One of these days I will kick the bucket and I want you to know which of my jewelry items are worth something.” However, we never addressed what she wanted as far as resuscitation or life-sustaining treatment. I didn’t realize the importance of the advanced directive and thus didn’t think to look for it. When she had that discussion with the neurologist, the hospital kept her as a full code since she did not clearly state that she did not want resuscitation in her advanced directive.
In a Crisis, Rational Thinking Can Often Go Out the Window
When I arrived at the hospital that day, I saw my mom’s hospital bed being rushed down the hall as the doctors and nurses worked diligently to revive her. My mom’s oncologist met me in the hallway and told me they were able to revive her, much to her surprise. However, in a short time, my mother’s organs began to fail, and she was placed on a ventilator to breathe for her. The oncologist came back out and told me there was no way for my mom to survive without the ventilator, as all her organs had shut down.
The doctor asked my permission to turn the ventilator off, and I agreed. I was in such a state of shock throughout the entire process, I couldn’t think straight. It was all happening so fast. How could I make life and death decisions while in a state of shock? How could I know what was the right thing to do? It felt completely surreal. How could this be happening?
‘Planning Is a Gift to Your Loved Ones’
As a Licensed Clinical Social Worker working with seriously ill individuals to do Advance Care Planning, I often think back to that time. This is part of the reason why I am so passionate about the benefit of everyone making these choices early on, before the unpredictable crisis happens.
The Advance Directive for Medical Care is so important, to select who you want to speak for you if you can’t speak for yourself, and to choose which life-sustaining treatments you want or don’t want. But the conversation, about the Advance Care Plan as a whole, is as important, if not more.
Sit down to talk with the person or people you choose to be your health care proxy. Talking about what’s important to you and when you want to say enough is enough. Or if you want to do everything possible until the end. Or somewhere in between. It’s a personal choice; it keeps you in control when you can’t speak for yourself. And it’s a gift to your loved ones, so they are not left wringing their hands wishing they knew what you wanted.